A federal agency resolves religious discrimination complaints about restrictions on clergy hospital visits.
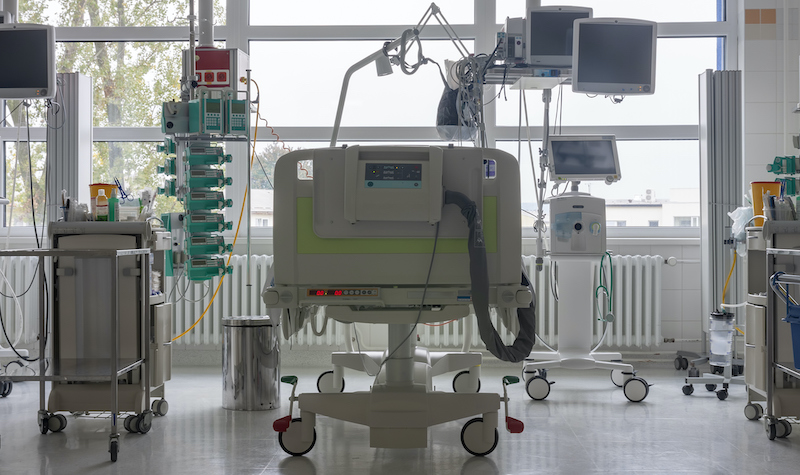
The COVID-19 pandemic has prevented patients from accessing their clergy in the midst of stressful and end-of-life situations. Hospitals seeking to restrict visitors face a difficult choice between infection control and enabling patients to receive social and spiritual support.
Responding to this tension, the U.S. Department of Health and Human Services (HHS) Office for Civil Rights has resolved religious discrimination complaints about restrictive hospital visitation policies. HHS has also worked with hospitals to develop protocols that can accommodate both infection prevention practices and patients’ free exercise of religion.
The HHS office, which possesses the legal authority to advise, investigate, and punish health care entities under certain federal nondiscrimination laws, has grappled with complaints of religious discrimination that have emerged during the pandemic. For example, a recent press release from the HHS Office for Civil Rights’s Conscience and Religious Freedom Division describes how the office has resolved complaints against hospitals by helping them develop appropriate visitation policies:
- In Maryland, a mother with COVID-19 was separated from her newborn son after giving birth alone. Shaken by the separation, she requested to have a priest visit the hospital and baptize her newborn child, but the MedStar Health System hospital denied the request.
- In Virginia, the family of a dying COVID-19 patient at Mary Washington Healthcare requested that a priest provide religious sacraments to the patient. The hospital denied the request. Only after learning that the Diocese of Arlington had filed a complaint with HHS did the hospital allow the priest to visit, in light of the patient’s end-of-life circumstances.
- Later, Mary Washington Healthcare denied another family’s request for a priest to provide religious sacraments to a patient. This time, the patient did not have COVID-19 and was not suspected of having the disease. The patient was in the intensive care unit, however, and the hospital had designated the entire unit as a COVID-19 unit. Because the hospital did not determine that the patient was in an end-of-life situation, it denied access to clergy visitation. The Diocese of Arlington again filed a complaint against the hospital.
In response to these complaints, HHS provided technical assistance to the hospitals on how to ensure adequate and lawful access—in accordance with federal statutes protecting individuals and institutions from religious discrimination—to chaplains and clergy during the pandemic. The agency based its assistance on a guidance document from the Centers for Medicare and Medicaid Services (CMS).
CMS describes multiple strategies for mitigating COVID-19 transmission in hospitals. The agency recommends limiting visitors for patients who have or may have COVID-19. Facilities should screen and educate visitors about infection prevention practices. If symptomatic visitors do not follow infection guidance, hospitals should restrict their presence in the facility.
The CMS COVID-19 document also references guidance from the Centers for Disease Control and Prevention, which provides hospital visitation recommendations as part of its COVID-19 infection control guidance. The recommendations include limiting visitors to those essential for the patient’s physical or emotional well-being and care, having visitors wear facemasks, and encouraging alternative patient-visitor interactions through video and phone calls.
CMS specifies, however, that patients must have adequate access to chaplains or clergy. Visitation policies must conform with two federal laws protecting religious exercise: the Religious Freedom Restoration Act, which restricts federally funded programs from substantially burdening the exercise of religion, and the Religious Land Use and Institutionalized Persons Act, which protects individuals and religious institutions from discrimination. CMS also requires that hospitals have written policies delineating clinically necessary or otherwise reasonable restrictions on the ability to visit patients.
With assistance from HHS, the MedStar Health System revised its COVID-19 visitation policy to conform with federal guidelines. Its new policy allows patients to receive religious service visits at “any reasonable time” that does not disrupt care.
Likewise, Mary Washington Healthcare in Virginia updated its policy so that patients in designated COVID-19 units can receive clergy visits, so long as the clergy member first completes scheduled infection control training, uses fit-tested personal protective equipment, and signs an acknowledgement of risks. In end-of-life and other extraordinary situations, clergy members may visit patients but must self-quarantine for 14 days after the visit.
Researchers point out that hospital visitors can contribute to COVID-19 viral shedding even when the visitors are asymptomatic. This fact necessitates rigorous surveillance and protective measures during visitation. Results from a study published in 2018 indicate that visitor restriction policies can contribute to a 37 percent reduction in hospital-acquired respiratory viral infections.
Developing the right visitation policies, however, requires consideration of several ethical principles, including protecting the public from harm and respecting individual liberty. In one study, researchers note that hospital visitation policies adopted in response to COVID-19 tend to be opaque and varied. The scholars recommend that hospitals adopt more transparent processes for granting exceptions to visitors, as well as greater stakeholder involvement in developing visitation policies during the pandemic.
“Compassionate care requires treating the body without sacrificing the soul,” said Roger Severino, director of the HHS Office for Civil Rights.



