Policymakers around the world are determining how to apply existing regulations to 3D organ printing.
When Selena Gomez suffered from Lupus, her best friend Francia Raisa donated her kidney to her, saving Gomez’s life. For decades, people just like Gomez have escaped death due to heroic organ donations, either from living or deceased donors.
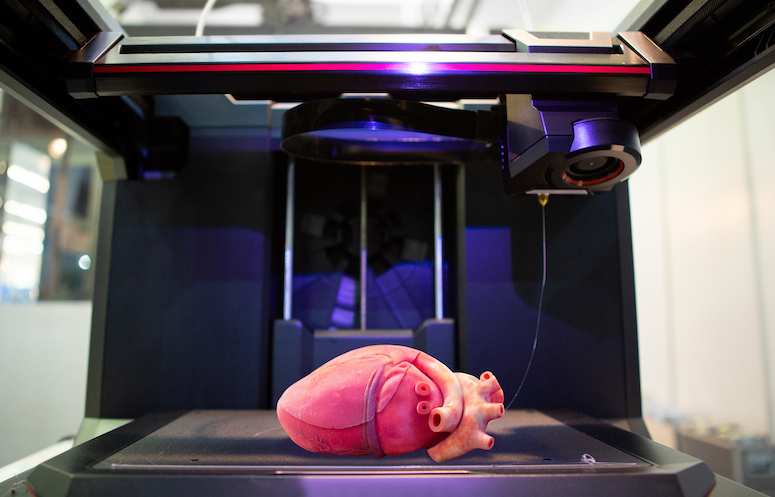
Today, 3D printing—also referred to as 3DP—may revolutionize the practice of organ donation. Although 3D printing is currently used to make jewelry, food, and art, it may soon be used for medical solutions such as organ donations and bionic limbs.
As a result, policymakers around the world seek increased regulation of 3DP organs. Yet 3D bioprinting does not clearly fit into existing regulatory frameworks.
Since bioprinting generally falls within the regulatory domain of “regenerative medicine, medical devices, and biologic drugs,” regulators face the challenge of applying existing rules to this uncertain field. As of now, it is unclear whether policymakers can effectively regulate bioprinting under existing regulations, or if a new, specific regulatory process will be necessary.
In determining how to regulate 3D organ printing, policymakers must juggle many possible concerns. Since the technology is still developing, a lot of uncertainty remains about what the actual risks and ethical concerns are. For example, one ethical concern is that 3DP organs may be available to wealthy people only, while less affluent individuals will be blocked out from using these organs.
Another concern is safety. Since 3DP may require stem-cell technology, and the patient’s own cells may be used for replication, it is difficult to assess the safety risks. Stem-cell therapy cannot be tested on a large sample of healthy people, which limits effective clinical analysis. Also, 3DP biotechnology may open up new uses beyond 3DP organs, such as enhancement of human capacities for military use. Developers could use the technology to make military officers or even terrorists less vulnerable to injury in battle, but this would open up a whole new challenge for law enforcement and national security.
The U.S. Food and Drug Administration (FDA) focuses on the regulation of 3D printed organs. FDA so far has only released guidance on 3DP, and the recommendations do not cover bioprinting.
A significant concern in the United States is that 3D printed organs do not fit into any clear category of law. First, they are not organs because they are not “born alive at any stage of development.” Second, they are not drugs because drugs are used orally rather than through an invasive surgery, and drugs are primarily meant to relieve illness while donated organs may completely cure an illness.
Some policymakers in the United States propose regulating 3DP organs as a “biological product,” defined as “a virus, therapeutic serum, toxin…or analogous product…applicable to the prevention, treatment, or cure of a disease or condition of human beings.”
Research company Biogelx suggests that biological products may be a promising category for printed organs. Within biological products, a 3DP organ is comparable to proteins because to print the organ, clinicians replicate healthy human cells, which include such proteins, says Biogelx. Although existing regulatory frameworks often compare 3DP organs to medical devices, Biogelx asserts that these organs should not be regulated as medical devices. Medical devices are not made of biological material and are often metal or plastic devices that help an individual’s standard of life, but 3DP organs are different since they cause a chemical reaction in the body and have the purpose of wholly replacing an existing organ, says Biogelx.
International policymakers are also struggling to find a sufficient regulatory framework. In Canada, Health Canada released draft guidance last year to develop regulations for medical device manufacturers working towards bioprinting. Health Canada has several concerns about bioprinting, and it suggests that manufacturers looking for bioprinting licenses should be required to submit information regarding the use of additives in materials, the verification of the software for the bioprinting design, the method of sterilizing the machines, and the process of safe removal and reuse of bioprinting materials and residues.
Finally, Europe’s 3DP health technology is regulated by the European Medical Devices Directive, the Active Implantable Medical Devices Directive, and the Invitro Diagnostic Medical Devices Directive. The Medical Devices Directive categorizes bioprinting devices into several risk classes. Across the different classes, devices ranked as higher risk are subjected to third party assessment and more “stringent” requirements for clinical data. The highest risk class, implantable devices such as 3D organs, requires an “independent design dossier review.” A design dossier assesses risk, evaluates clinical data, and demonstrates the technology’s compliance with regulations and requirements.
Although 3D printing of organs is right around the corner, policymakers around the world lack the information necessary to make regulatory decisions in this space. Different countries have different approaches, but many of the leading nations in 3DP share similar concerns. With more information, regulators will have to decide if existing regulatory frameworks can adequately address the safety concerns of 3D printed organs.



